[ad_1]
Medical claims include codes for different key entities involved like the patient, provider, and billing service. An “entity code rejection” happens when one of these codes is invalid. This could be because it’s missing, expired, or simply incorrect. For example, if the patient’s ID code is outdated or the provider’s NPI number is wrong, the claim will be rejected. Resubmitting the billing claim requires correcting whichever entity code caused the rejection.
In most cases, wrong billing NPI (the equivalent of Box 33 on the CMS-1500) or incorrect Tax ID given in Box 25 on the claim leads to the entity code rejection error when submitting a medical claim.
Reasons for Entity Code Rejection
Let’s discuss some of the most common reasons for entity code rejection in medical billing, including wrong payer ID, expired or invalid entity codes, mismatched claim data with codes, incomplete insurance provider information, and claims for newborn patients. By understanding these reasons, healthcare providers can take steps to prevent claim rejections and ensure that their claims are processed correctly.
DID YOU KNOW?
The quicker an entity code error is identified and corrected, the faster the claim can be resubmitted. This improves the cash flow of a provider.
1). Wrong Billing NPI
When submitting a medical claim, the billing provider’s National Provider Identifier (NPI) number must be accurately entered in Box 33a of the CMS-1500 form. This unique 10-digit code identifies the individual or organization that will receive payment for the services rendered.
If an incorrect or invalid NPI is given, payers will often reject the claim due to this entity code error. Verifying that the billing NPI matches the provider’s active, federally-issued number is an essential step to avoid entity code rejection.
With the proper NPI in place, the relationship between provider and claim can be reliably established.
2). Incorrect Tax ID given in Box 25
Medical claims include the tax identification number of the billing provider in Box 25 of the CMS-1500. Whether using an Employer Identification Number (EIN) or Social Security Number (SSN), this ID must precisely match the number under which the provider files taxes.
When an inaccurate tax ID is submitted, payers cannot verify the provider’s identity. The resulting entity code rejection halts the claims process until the proper tax ID can be entered. Careful review of this business identification number prior to submission helps bypass entity errors.
With the right tax ID in Box 25, the path is cleared for claims to reach approval based on correct provider information.
3). Incorrect Payer ID
The payer ID is a unique identifier for insurance companies that process claims. If this ID is input incorrectly, the insurance company might not recognize it. As a result, the claim will not be processed as intended, leading to its rejection.
4). Mismatched Claim Data with Codes
The details provided in the claim must align with the specific codes used. If there’s a discrepancy or mismatch, the insurance company can interpret this as an error, possibly rejecting the claim.
5). The Patient is a Newborn
Sometimes, when a baby is born, they might not be immediately added to their parent’s or guardian’s insurance policy. The claim may be rejected if a claim is made for medical services for the newborn before they are added to a policy.
DID YOU KNOW?
A single claim rejection might not seem like a big deal, but when these add up, the financial implications for a practice can be significant. Additionally, consistent mistakes could flag your practice for potential audits by insurance companies or regulatory bodies.
Steps to Fix Entity Code Errors
There are several steps that healthcare providers can take to fix entity code rejections. These include verifying payer information, properly checking entity codes, matching claims data with codes, submitting complete provider information, and utilizing EHR software.
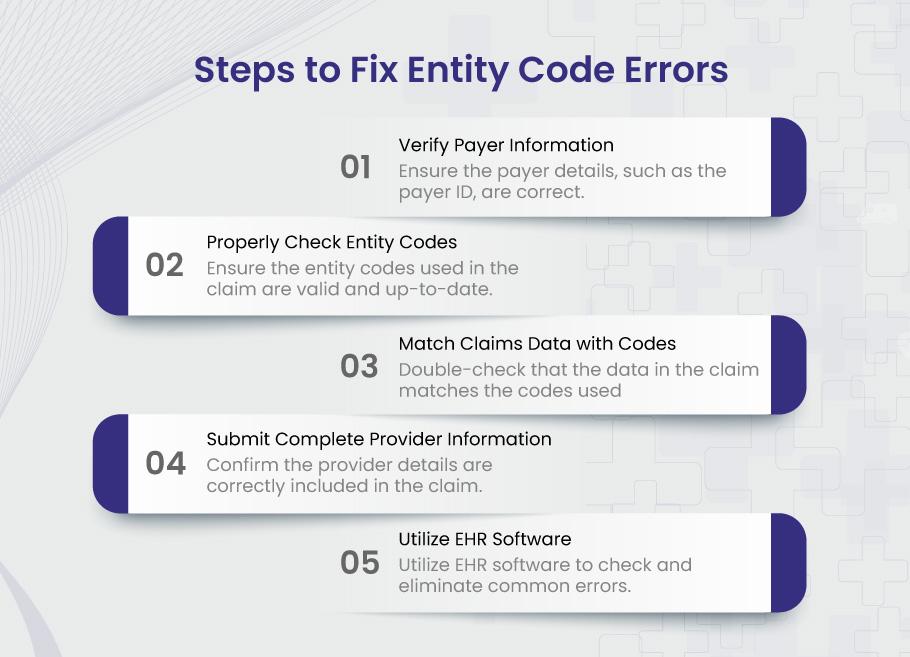
1). Verify Payer Information
Before submitting a claim, one should ensure that all details related to the payer, such as the payer ID and other relevant information, are correct. This can help prevent rejections due to incorrect details.
2). Properly Check Entity Codes
Before submission, it’s essential to ensure that the entity codes used in the claim are valid and up-to-date. This reduces the chance of using an expired or invalid code.
3). Match Claims Data with Codes
Double-checking that the data in the claim (like services provided) matches the codes used is crucial. This can prevent rejections due to mismatched data.
4). Submit Complete Provider Information
All the necessary details about the provider, like NPI, should be thoroughly checked and included in the claim. This ensures that no missing or incomplete information might lead to rejection.
5). Use a Healthcare Clearinghouse Software
Resubmitting claims due to entity code rejections wastes time and money. Using a clearinghouse software eliminates this problem. The clearinghouse automatically validates all codes for the patient, provider, and the 3rd party billing company against up-to-date databases. Invalid or expired codes are caught and corrected pre-submission. You avoid rejections altogether.
Some medical billing companies, like BellMedEx, offer their customers a full clearinghouse free of charge. Our healthcare clearinghouse software saves you time and ensures first-time acceptance.
Pro Tips:
1. Ensure consistent and standardized documentation processes across your practice. This minimizes errors and discrepancies that could trigger entity code rejections.
2. Train staff members on the latest billing codes, guidelines, and software updates. This proactive approach can help catch mistakes before they lead to rejections.
3. Schedule regular internal audits of your billing process. This helps identify patterns or recurring mistakes, allowing you to address them systematically.
FAQs
1. What is an entity code rejection in medical billing?
An entity code rejection occurs when incorrect information regarding the entities involved in the medical billing process occurs. This can pertain to the patient, the provider, or the 3rd party medical billing service, resulting in a rejected medical claim.
2. Why is it crucial to prevent entity code rejections?
An entity code rejection can lead to claim denials, meaning that the healthcare practitioner might not get paid for their services. This can result in time and revenue loss, negatively affecting the practitioner’s financial stability.
3. How can healthcare providers avoid or rectify entity code rejections?
Providers can avoid these rejections by verifying payer information, ensuring entity codes are valid, matching claims data with codes, submitting complete provider data, and using a medical Clearinghouse software like FusionEDI, which can assist in reducing common claim submission errors.
4. What is an entity code rejection in Medicare?
An entity code rejection in Medicare means that the provider’s National Provider Identifier (NPI) number or Tax ID number used on the claim form does not match the information Medicare has on file for that provider. This causes the claim to be rejected. To resolve, the provider must verify their NPI and Tax ID are correct on the claim form before resending it.
5. What is the difference between provider entity rejection and provider claim rejection??
An entity code rejection means there is an error with the provider’s identifying information on the claim form – typically their NPI number or Tax ID. This results in the claim being rejected only on the basis of invalid provider details. The services billed may be perfectly valid otherwise.
A claim rejection is much broader – it means there is a problem with the actual services or charges listed on the claim. This could be an unrecognized procedure code, mismatch with the diagnosis, services not covered by the patient’s plan, or any other detail specific to that billed encounter. The whole claim is rejected, not just the provider’s identifying details.
In summary, entity code rejections relate specifically to provider identification numbers, while claim rejections pertain to the services, charges, and other billing details on the claim itself. Entity code issues are usually quick fixes, while claim rejections often require deeper investigation to resolve. Knowing the difference helps providers address rejections properly.
[ad_2]





