Medical claim forms are an essential component of the medical billing process.
In simpler terms, a medical claim form is a formal written request that a healthcare provider submits to an insurance company, Medicare or Medicaid, or another affiliated entity seeking compensation for the healthcare services provided to a patient.
Healthcare providers firmly believe that their patients are entitled to specific rules or statutes of insurance companies, and the medical claim form serves as a legal document that justifies the request for compensation.
The medical claim form is an important medical billing documentation tool serving multiple stakeholders, including patients, insurance companies, and healthcare providers.
🧑🏻 For patients, it ensures that their healthcare expenses are covered by their insurance providers, providing them with financial security.
⚕️ For insurance companies, it serves as evidence of the services rendered to the patient, allowing them to process the claim efficiently and accurately.
🩺 For healthcare providers, the medical claim form is essential for receiving payment for the services they provide.
The Types of Medical Claim Forms Used in the US Healthcare System
The US healthcare system relies heavily on medical claim forms to process reimbursement requests for services rendered by healthcare providers. These forms capture essential information about the patient, service details, diagnosis, and charges.
Here’s an overview of some common types of medical claim forms used:
- Institutional Claim Form (includes 837I, UB-04 Form)
- Professional Claim Form (includes CMS-1500, 837P)
- Dental Claim Form (includes ADA Dental Claim Form J400, 837D)
1). Institutional Claim Form
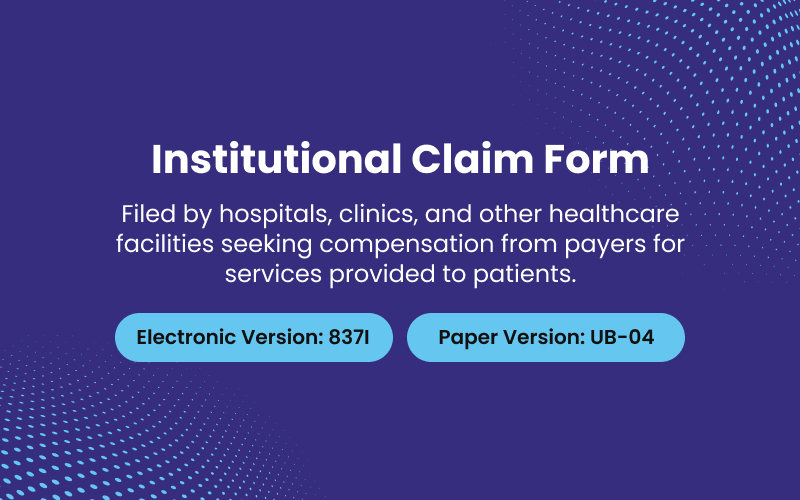
Institutional claims are claims that are filed by hospitals, clinics, and other healthcare facilities—rather than individual healthcare providers such as physicians or nurses—to seek compensation from insurers and other payers for services provided to patients. This claim form provides a comprehensive snapshot of the patient’s medical history, the services they received, and the associated costs.
⇉ Types of Institutional Claim Forms
When it comes to institutional claim forms, there are two main types used by institutional providers – electronic and paper.
The most common electronic form nowadays is the 837 Institutional (837I), which follows a standard format for sending claims electronically. This allows for faster processing compared to paper. The old paper standard was the UB-04, also called the CMS-1450. It’s still used sometimes if the provider can’t submit electronically.
The 837I is best for routine claims that don’t need attachments or extra documentation. It’s fast and efficient. The UB-04 is good for claims that are out of the ordinary or need paperwork included. It’s a bit slower but works when electronic isn’t an option.
Both serve a purpose – one for typical claims sent online, one for special cases submitted by mail. But in general, electronic 837 Institutional claims are the new normal for institutional providers.
2). Professional Claim Form
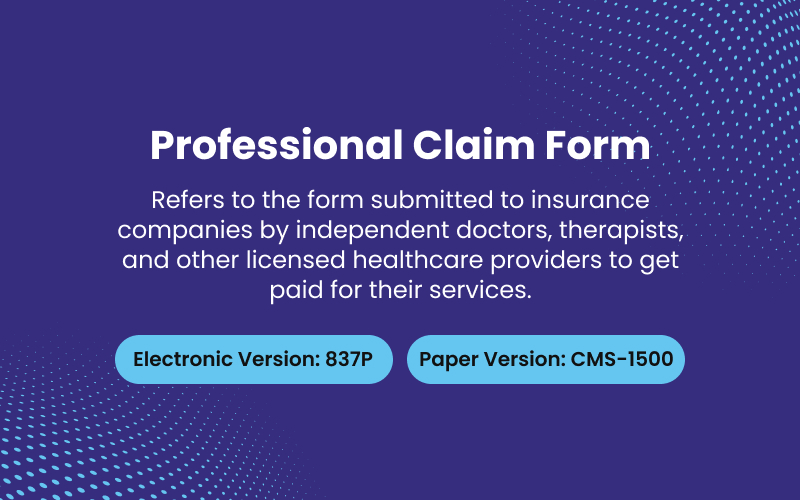
Professional claim forms refer to the bills submitted to insurance companies by independent doctors, therapists, and other licensed healthcare providers. The professional providers themselves are the physicians, physical therapists, psychologists and so on who work directly with patients. To get paid for their services, they fill out professional claim forms with information like the dates of treatment, services provided, and total charges for each patient. The insurance companies then decide how much they will reimburse.
⇉ Types of Professional Claim Forms
When it comes to professional medical claim forms, there are two main types – electronic and paper.
The most common electronic form is the 837 Professional (837P) claim form. This follows the ANSI ASC X12N standard for healthcare transactions, just like its cousin, the 837I institutional form. It allows for efficient, standardized electronic submission of claims data.
The old school paper claim form is the CMS-1500. This has traditionally been used by doctors, clinics, and other professional providers to submit claims by mail. It contains all the required data fields and codes needed for reimbursement.
The 837P is ideal for practices with a high volume of claims. It’s fast, accurate, and integrates directly into practice management and billing systems. The CMS-1500 is the way to go for providers who prefer paper or have a low claim volume. While one is pixels and one is pulp, both serve the same essential purpose – getting providers paid for services rendered.
3). Dental Claim Form
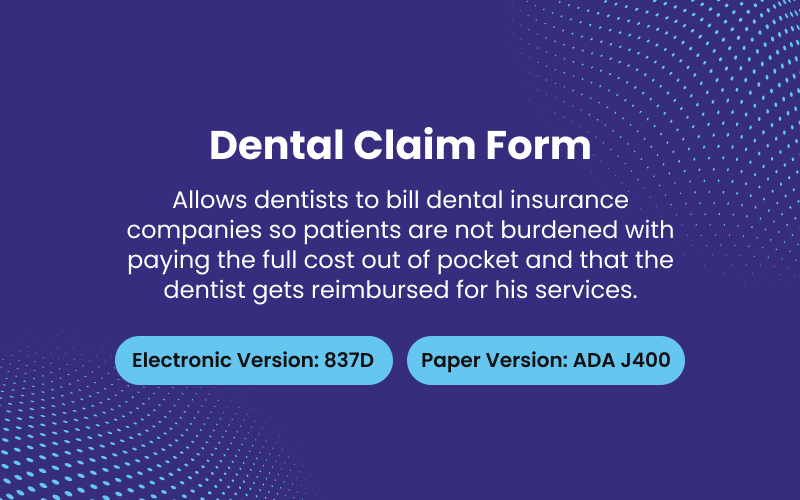
In the United States, when a patient visits their dentist for any treatment, the dentist will submit a claim to the patient’s insurance provider for the services rendered. This is done using a standard form called a Dental Claim Form. Unlike a medical claim form, a dental claim form is specifically designed to provide details about dental procedures and care.
The goal of a Dental Claim Form is simple: to allow dentists to bill dental insurance companies so patients are not burdened with paying the full cost out of pocket and that the dentist gets reimbursed for his services.
The Dental Claim Form provides details such as the patient’s name and insurance details, the date of service, descriptions of the procedures performed, the charges for each service, and the total amount due. The dentist submits the claim form to the patient’s insurance provider. The insurance provider then processes the claim and pays their share of the cost, while the patient pays any remaining amount as required by their insurance plan.
Without dental claim forms, dentists would have significant difficulties receiving payment and patients would face much higher out-of-pocket costs.
⇉ Types of Dental Claim Forms
There exist two primary types of forms utilized for submitting dental insurance claims.
The first is referred to as the ADA Dental Claim Form J400. This standardized form, created by the American Dental Association, is employed when a patient requires dental treatment and their dentist needs to bill the insurance provider to receive reimbursement for services rendered.
The specifics of the treatment, including procedures done and their associated fees, are documented on the form which is then forwarded to the insurance company by either mail or electronic means.
The second type of claim form is designated as the 837D. This form is also used to report dental treatments and request payment from insurance companies. However, the 837D is in an electronic format following the HIPAA standard.
Dentists enter the required patient and treatment information into their practice management software which then generates the electronic 837D claim form. This is most often transmitted directly to insurance providers for processing the reimbursement.
To summarize, the ADA Dental Claim Form J400 is a paper form used for basic dental insurance claims while the 837D is an electronic form serving the same purpose but in a digital format consistent with HIPAA regulations.
The J400 continues to be accepted by many insurance companies but the 837D is becoming more widely utilized due to its efficiency and standardization. Both fulfill the necessary task of communicating to insurers the specifics of dental care provided so that dentists can be properly reimbursed.
Anatomy of Medical Claim Forms
Each form has these essential sections:
- Patient Information [Demographics like name, date of birth, and insurance ID].
- Provider Information [Physician or facility details].
- Procedure Information [Diagnosis codes and details about the service provided].
- Charges [The cost of the service(s)].
- Insurance Information [Your insurance details and policy number].
The Key Attributes of a Medical Claim Form
| Field | Description |
| Code | The unique code for this claim form |
| Description | The description for this claim form |
| Insurance Type | The insurance type for this claim form |
| Claim Form Type | Optional reference to claim form type |
| Procedure 1 usage name | The attribute name in dynamic logic |
| Procedure 1 definition | Flex Code System that defines which codes can be entered |
| Procedure 1 fatal non match indicator | If checked, a non match leads to a fatal system message. If not, an informative message is applied instead |
| Procedure 2 usage name | The attribute name in dynamic logic |
| Procedure 2 definition | Flex Code System that defines which codes can be entered |
| Procedure 2 fatal non match indicator | If checked, a non match leads to a fatal system message. If not, an informative message is applied instead |
| Procedure 3 usage name | The attribute name in dynamic logic |
| Procedure 3 definition | Flex Code System that defines which codes can be entered |
| Procedure 3 fatal non match indicator | If checked, a non match leads to a fatal system message. If not, an informative message is applied instead. |
➤ When it comes to processing medical claims, there’s a step where the system automatically matches procedure codes. If the codes don’t match up, a fatal non-match indicator is triggered. But don’t worry, this indicator can’t be used to enter a fake code on the claims page or send one through the claims update integration point.
➤ Every claim form belongs to a specific type of insurance. The type of insurance determines what part of the business it is for, like car insurance, health insurance, or travel insurance.
➤ Each claim form can only belong to one claim form type. We use claim form types in many of our rules to refer to groups of claim forms.
➤ A good example for health insurance in the US is that claim forms represent the different ways a claim can be submitted. This includes electronic formats 837P, 837I and 837D and paper forms UB04, CMS1500 and J400.
➤ When it comes to two specific claim forms, the UB04 and the 837I, they’re both considered institutional claims. This means they’re treated the same way for adjudication purposes, regardless of whether they were submitted electronically or through the mail. In other words, both forms would fall under the umbrella of the “Institutional” claim form type.
Top 10 Tips to Fill Out Medical Claim Forms
1). Check that you have the correct patient and insurance information. Make sure the patient’s name, date of birth, insurance ID number and group number are all accurate. Double check the insurance payer’s mailing address for claims. One small error can lead to denied or delayed payments.
2). Use the proper claim form. Choose between the CMS 1500 or UB04 form depending on the type of provider you are. Make sure you are using the most up to date version of the form to avoid rejections.
3). Record the proper diagnosis and procedure codes. Check that the ICD-11 diagnosis codes and CPT procedure codes you’ve selected accurately reflect the services provided. Code correctly the first time to avoid delays.
4). Include documentation to support your claim. Attach operative reports, progress notes, and other records to provide evidence for the medical necessity of the services billed. Lack of documentation is a leading cause of claim denials.
5). Check that your fees are within the allowed amount. Bill your usual and customary fees unless the insurance payer has a pre-negotiated rate. Charging above the allowed amount will result in payment delays and unhappy patients.
6). Obtain preauthorization when required. Some insurance plans require preauthorization for hospital admissions, procedures, and other services. Failure to obtain preauthorization can result in denied claims.
7). Meet timely filing deadlines. Submit claims within 30-90 days of the date of service depending on the insurance payer’s requirements. Late submissions will lead to denied claims.
8). Submit electronically whenever possible. Electronic submissions through a clearinghouse help to reduce errors and allow for faster processing and payment. Only use paper claim forms when electronic filing is not an option.
9). Follow up on unpaid claims. Check the status of unpaid claims after 30 days. Look for denials or requests for additional information. Resubmit or appeal denied claims as needed. Don’t leave money on the table due to lack of follow up!
10). Keep good records. Maintain copies of all claims, correspondence, and remittance advice for reference. Well-organized records make it easier to track the status of claims, identify trends, and resolve any issues.
Don’t know how to choose the correct claim form and fill it? Let Us Help You!

For healthcare providers, claim forms are a necessary evil. Choosing the right form, CMS 1500 or UB-04, is just the beginning. Enter one wrong code or missed signature and your reimbursement could be delayed or denied. Not to mention the penalties you could face for inaccurate claims.
Stop struggling with claim forms. ProcareMedex is here to help! Our medical billing specialists thrive on paperwork that makes most providers cringe. We’ll ensure your claims are filled out completely, correctly, and ready for prompt reimbursement. One less headache for your practice.
Trust us to handle the confusing claim forms. You handle the critical patient care. Contact us today so your claims sail through cleanly.





