The Medicare program has developed a new system to grade doctors on how well they treat their patients. It’s called the Merit-based Incentive Payment System or MIPS for short.
MIPS decides how much money Medicare will pay doctors for seeing people on Medicare. It looks at things like how healthy doctors keep their patients, how good a job they do taking care of illnesses, and what patients say about their doctors.
In 2024, MIPS scores will matter a lot. Doctors will get points for things like keeping patients healthy, properly managing diseases, and having good patient reviews. If a doctor scores well, Medicare pays them more. If they score poorly, Medicare pays them less.
This article explains MIPS in 2024 including who must participate, how scores are calculated, and how pay is adjusted based on those scores. For doctors, MIPS scores translate directly to how much they get paid, so performing well in MIPS is important business for them.
Introduction to QPP and MIPS
The Quality Payment Program (QPP) and the Merit-based Incentive Payment System (MIPS) work together to improve healthcare quality and outcomes.
The QPP was created by Medicare to reward high value, high quality care. MIPS is one part of the QPP that measures clinician performance across quality, cost, improvement activities, and promoting interoperability. MIPS scores determine payment adjustments under QPP.
So in simple terms, MIPS scores lead to QPP incentives. By participating in MIPS, clinicians can earn positive payment adjustments by scoring well. The higher the MIPS score, the higher the Medicare payment. This encourages clinicians to deliver better care. MIPS and QPP aim to tie Medicare payments to value and quality, rather than just quantity of services.
What is QPP?
The QPP stands for Quality Payment Program. It was established under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
The QPP dominates value over volume in delivering healthcare services. Its primary purpose is to improve Medicare by helping providers focus on care quality and the one-on-one patient relationships that lead to better health outcomes.
For example, under the QPP, a primary care physician is rewarded for spending more time with patients to fully understand their health conditions and provide preventative care, rather than simply treating illnesses as they arise.
The physician receives incentives for achieving better outcomes, like reducing avoidable hospital admissions, rather than being paid based on the number of office visits and procedures performed. This encourages the physician to focus on quality care.
The Quality Payment Program (QPP) consists of two major tracks:
- The Merit-based Incentive Payment System (MIPS)
- Alternative Payment Models (APMs)
What is MIPS?
The Merit-based Incentive Payment System (MIPS), established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), came into effect on January 1, 2017.
The way Medicare pays doctors these days depends a lot on how they measure up according to MACRA. MACRA takes a look at doctors individually or in their group practices and grades them on four areas:
👉 Quality Measures – Are patients getting good, high-quality care?
👉 Cost Measures – How much does it cost the doctor to provide that good care?
👉 Health IT Use – Is the doctor using technology properly in the office to keep records and share information?
👉 Practice Improvement Activities – Is the doctor constantly working to make the practice run more efficiently?
Doctors who score the best in these areas according to MACRA standards get paid more by Medicare. Those who don’t score as well may face lower payments.
MIPS acts as a catalyst for transforming the healthcare industry from fee-for-service to pay-for-value. Under the traditional fee-for-service model, providers are paid based on the quantity of services performed, regardless of outcomes. MIPS, on the other hand, ties Medicare payments to the quality of healthcare service provided by the provider to the patient and cost-efficiency.
So this would not be wrong to say that MIPS strives to transform Medicare into a purchaser of ‘Quality’ rather than ‘Quantity’.
Here’s how MIPS scoring works:
With MIPS, the idea was to take the Physician Quality Reporting System, which measured the quality of care through various metrics, the Value-based Payment Modifier, which adjusted Medicare payments based on performance, and the Electronic Health Record Incentive Program, which provided rewards for using electronic health records, and roll them all together into one consolidated program that would be easier for physicians and clinics to participate in.
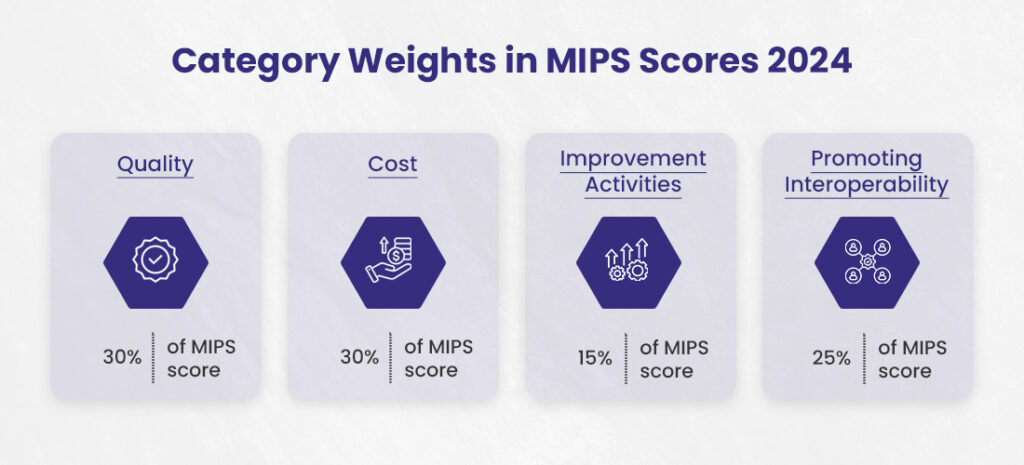
Eligible clinicians are scored on four weighted performance categories: quality (30%), cost (30%), promoting interoperability (25%), and improvement activities (15%) of the total score. Based on their composite performance score, clinicians receive positive, negative, or neutral adjustments to their Medicare Part B reimbursements.
MIPS Reporting Options
There are three MIPS reporting options for eligible clinicians:
1. Traditional MIPS
This is where most physicians report on certain measures of quality, resource use, clinical practice improvement activities, and advancing care information. Based on how you score, you may earn a bonus, face no change in pay, or get a small penalty.
2. Alternative Payment Model (APM) Performance Pathway (APP)
This is for doctors already in approved Alternative Payment Models set up by Medicare. These are special programs where doctors take responsibility for both the cost and quality of care for their patients. Medicare evaluates just two categories for these doctors: quality of care and cost of care. The requirements are more flexible for doctors in these models.
3. MIPS Value Pathways (MVPs)
This pathway ties measures and activities together around a specific medical condition or procedure. The idea is to align what doctors report more closely with how they actually practice medicine. Medicare is still developing many of these MVPs with input from doctors and medical experts. Doctors can choose to report through an MVP once they are ready if they think it suits their practice better.
| Comparison Among 3 MIPS Reporting Options | |||
| Feature | Traditional MIPS | APM Performance Pathway (APP) | MIPS Value Pathways (MVPs) |
| Year Established | First year of QPP | Not specified | Newest option |
| Designed For | General MIPS-eligible clinicians | Clinicians in a MIPS APM | Clinicians focusing on a specialty or medical condition |
| Measure Selection | Select from all finalized measures and activities | Predetermined measure set | Subset of measures and activities relevant to a specialty or condition |
| Promoting Interoperability Measures | Complete set required | Complete set required (same as Traditional MIPS) | Needed complete set (same as Traditional MIPS) |
| Cost Performance | Data collected and calculated by MIPS | Data collected and calculated by MIPS | Data collected and calculated by MIPS includes population health measures |
| Improvement Activities | Choose and report from a finalized list | Full credit automatically (evaluated annually) | Select and report on the reduced number (compared to Traditional MIPS) |
| Scoring Opportunities | Standard scoring based on performance in selected measures and activities | Designed to reduce reporting burden and create new scoring opportunities for MIPS APM participants | More meaningful groupings of measures and activities for a connected assessment of quality |
| Encouragement of APM Participation | No specific focus on APM participation | Encourages participation in APMs | No specific focus on APM participation |
Eligibility and Participation in MIPS Program
If you are an individual clinician who bills Medicare Part B, such as a physician, nurse practitioner, or physician assistant, you can participate in MIPS.
Eligibility is determined based on specific criteria set by Medicare, including providing care for more than 100 Medicare patients or billing more than $30,000 to Medicare Part B during a 12-month determination period. First-year Medicare providers and those meeting the low-volume threshold are exempt from participation.
Here are some participants of MIPS:
- Physicians (MD/DO, DDS, DDM, DPM, Optometrists, and Chiropractors)
- Osteopathic Practitioners
- Physician assistants
- Nurse practitioners
- Clinical nurse specialists
- Nurse midwives
- Clinical psychologists
- Dieticians/nutritional professionals
- Clinical social workers
- Certified nurse-midwives
- Certified registered nurse anesthetists
- Physical or occupational therapists
- Speech-language pathologists
- Qualified audiologists
Clinicians can choose their pace of participation, starting any time between January 1 and December 31 of the performance year, allowing flexibility to adapt to the Medicare Quality Payment Program (QPP).
There are 5 participation options: individual, group, virtual group, subgroup, and APM Entity. Use the QPP Participation Status Tool to view your eligibility status, which informs you of your participation options. You can also learn more about how QPP determines eligibility and the eligibility determination period and snapshots.
How to Check Your Participation Status for the Quality Payment Program of CMS?
First, get your 10-digit National Provider Identifier (NPI) code . You’ll need to enter that, along with which year you want to check – this year or maybe last year.
Once you’ve got that sorted, visit QPP’s Participation Lookup tool and look for where it says “check your participation status.” Click on that.
If you’ve never signed up for their QPP account, you’ll have to register for one. But if you already have an account, just log right in. Either way, you’ll end up on a page showing whether they’ve included you as one of the doctors getting bonuses or penalties under this here Quality Payment Program of theirs.
MIPS Categories and Scoring

MIPS includes four performance categories that are scored to calculate a composite performance score. Each category contributes a different percentage to the total score.
MIPS assesses performance scores in four categories:
1). Quality
Weight: Typically, this category contributes 30% to the overall MIPS score.
Scoring and Methodology: Healthcare providers must report on six measures of their choice, and scores are given based on performance benchmarks established by CMS (Centers for Medicare & Medicaid Services). Providers can earn up to 10 points per measure.
2). Cost
Weight: Usually accounts for 30% of the total score.
Scoring and Methodology: CMS calculates the score based on claims data, so no additional reporting is required from providers. Cost performance is evaluated through measures that assess the total cost of care during the year or hospital stay. The score reflects the resources used to care for patients and is compared against historical benchmarks and peer performance.
3). Improvement Activities (IA)
Weight: Generally makes up 15% of the MIPS score.
Scoring and Methodology: Providers select from a list of over 100 activities and report their participation. Activities vary in weight (medium or high), and providers must accumulate a set number of points to earn the total score for this category. This improves clinical practice, including care coordination, beneficiary engagement, and patient safety. There are high and medium-weighted activities, and clinicians choose the activities that best fit their practice.
4). Promoting Interoperability (PI)
Weight: Typically contributes 25% to the overall score.
Scoring and Methodology: This category focuses on using certified electronic health record technology (CEHRT) to manage patient care. Providers must report on e-prescribing, health information exchange, patient access, etc. Scores are based on performance for each measure. Clinicians must fulfill several objectives and measures, like e-prescribing and health information exchange.
Composite Performance Score (CPS) Calculation
The composite performance score (CPS) earned by a physician or provider can be calculated as formula given below:
MIPS CPS Max Score = 100 points
Final MIPS Score = Quality Weighted Score (30%) + PI Weighted Score (25%) + IA Weighted Score (15%) + Cost Weighted Score (30%) + Complex Patient Bonus (if applicable) + Small Practice Bonus (if applicable)
Rewards for MIPS Performance Scores
The MIPS system is designed to reward high-performing clinicians to improve the overall quality of healthcare:
- Above 75 Points: Clinicians with an MIPS performance score above 75 typically receive a substantial positive payment adjustment. As of the most recent guidelines, this could be as high as 9% of their Medicare Part B reimbursements.
- Below 75 Points: Those scoring below 75 may receive a minor positive adjustment, no adjustment, or even a negative adjustment, depending on their specific score relative to the performance threshold.
MIPS Penalties and Bonuses
- Penalties: Clinicians scoring significantly below the threshold risk may receive a penalty, which decreases their Medicare reimbursements.
- Bonuses: Additional incentives, such as the exceptional performance bonus for top performers, further enhance the positive adjustments for the highest scorers.
Incentives for Participating in an Advanced APM
Advanced APMs offer a different set of incentives aimed at encouraging providers to take on more risk and responsibility for patient outcomes:
- 5% Incentive Payment: Participants in qualifying APMs can receive a lump sum incentive payment of 5% of their estimated Part B covered professional services for the previous year.
- Exemption from MIPS: Providers sufficiently involved in an Advanced APM are exempt from the MIPS reporting requirements and payment adjustments.
These frameworks are part of a broader move towards value-based care, where providers are financially incentivized to improve the Quality and efficiency of healthcare rather than the volume of services delivered.
MIPS Payment Adjustments 2024
The CMS sets the performance threshold for 2024, and clinicians’ final scores determine the payment adjustments they will receive. Providers can see positive, negative, or neutral payment adjustments depending on their MIPS final score.
For 2024, an MIPS performance score above 75 could reward providers with up to a 9% increase in Medicare reimbursements, reflecting their commitment to high-quality care.
Conversely, scores below the threshold may result in penalties, reducing Medicare payments. The program is designed to be budget-neutral, which means penalties fund the bonuses. For example, if Dr. Jones gets an 80 and gets a bonus, but Dr. Smith gets a 70 and gets penalized, it’ll balance out for Medicare’s budget.
➜ Check out this CMS User Guide to learn more about MIPS Payment Adjustments 2024 and MIPS Performance Score.
The Importance of Certified EHR Technology (CEHRT) for MIPS Reporting in 2024
If you’re going to run a medical practice these days and get proper compensation from Medicare for your services, you’re going to need an electronic health records system that’s up to snuff. Medicare calls these certified electronic health record technologies or CEHRT.
CEHRT refers to electronic health records systems that fulfill the specific requirements laid out by Medicare and Medicaid and the Office of the National Coordinator for Health Information Technology. These requirements ensure that the systems help doctors provide high-quality care, keep patients’ information private and secure, and can exchange information with other systems.
CEHRTs are key to getting scored right in Medicare’s Merit-based Incentive Payment System. MIPS evaluates how well doctors care for their patients, and having a CEHRT that meets Medicare’s standards is critical to getting a good MIPS score. A good MIPS score means better pay from Medicare.
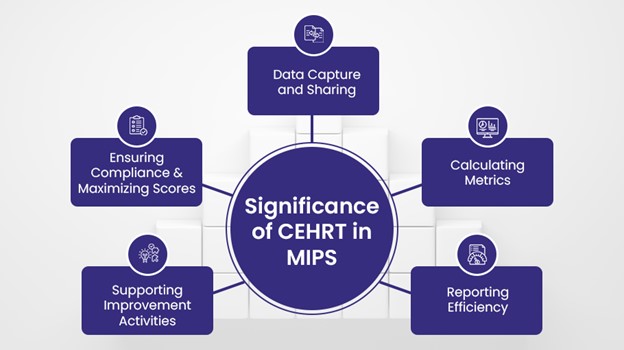
CEHRT is essential in MIPS for several reasons:
✅ Data Capture and Sharing
One of the primary ways in which CEHRT is used in MIPS is through its ability to capture and share data across various healthcare systems. This is essential for ensuring that patient data is easily accessible to healthcare providers, regardless of where they are located. With CEHRT, patient data can be shared in real-time, allowing for faster and more accurate decision-making.
To illustrate the importance of CEHRT in MIPS, let’s consider an example. Say a patient visits their primary care physician for a routine check-up, and the physician identifies a potential health issue that requires a specialist’s attention. With CEHRT, the primary care physician can quickly and easily share the patient’s medical records with the specialist, who can then make an informed decision about the patient’s care.
Of course, with the sharing of patient data comes concerns about security and privacy. CEHRT is designed with built-in security features to safeguard patient data, and it must meet certain interoperability and functionality requirements to ensure that data can be easily shared among various healthcare systems.
✅ Calculating Metrics
CEHRT is pretty handy for the Merit-based Incentive Payment System. It’s because it gathers up all your patient information and then crunches the numbers to measure your performance. It looks at things like how many of your patients with diabetes got their blood sugar tested or how many ladies came in for their mammograms. The computer tallies it all up automatically so you don’t have to do it yourself with paper and pencil.
With the CEHRT figuring the metrics for you, reporting for MIPS becomes a breeze. You just review the calculations, make sure they look right, and then send them off. The MIPS agents use those metrics to evaluate how you did over the year and determine your MIPS score. A good score means you get a bonus in your Medicare payments. The CEHRT streamlines the whole MIPS process so you can focus on doctoring instead of pushing paper.
✅ Proper Reporting Efficiency
Without CEHRT, medical practices won’t be able to properly report the necessary measures to CMS and qualify for the MIPS incentive payments. CEHRT is essential for MIPS because it provides an efficient way to collect and report the data that demonstrates a practice is providing high-quality care.
Using an electronic health record system, physicians and their staff can easily track things like patient outcomes, care coordination, patient safety and patient satisfaction. At the end of each performance year, they can then compile all this data to report to CMS and show they have earned the MIPS incentive payments.
✅ Supporting Improvement Activities
MIPS rewards physicians based on four performance categories, one of which is Improvement Activities. This measures how providers are improving care through activities focused on patient safety, care coordination, population management, and more.
To receive credit for the Improvement Activities performance category, clinicians must attest that they have completed certain activities using CEHRT. This could involve providing patient access to EHRs, sharing information electronically with public health agencies, participating in a quality improvement registry, and so on. CEHRT offers the functionality and interoperability required to successfully carry out these improvement initiatives.
Without certified EHR systems, practices would struggle to meet the criteria for this important MIPS component.
✅ Ensuring Compliance and Maximizing Scores
With a CEHRT system, providers can seamlessly track quality measures and report data to Medicare. This takes a huge compliance burden off their shoulders. No more manual chart reviews or spreadsheet gymnastics. The CEHRT system does that heavy lifting for them. Ultimately, this frees up time for patient care while ensuring accurate MIPS reporting.
The CEHRT optimizes and maximizes MIPS scores too. It can uncover care gaps in patient panels and suggest appropriate interventions. Providers using CEHRT often have higher scores on quality measures than those without. The system provides built-in clinical decision support that facilitates evidence-based care. This directly translates into more MIPS points.
Optimize Your MIPS Scores with ProcareMedex
As a medical billing company, we offer a comprehensive Physician Billing Service that not only handles full service billing with RCM and denial management, but also optimizes a physician’s MIPS scores.
How do we do this, you ask?
Well, our process ensures that physicians gain MIPS positive reimbursements and bonuses by staying up-to-date with the latest regulatory requirements, tracking performance data, and submitting accurate and timely reports.
In addition, our EHR system is specifically geared towards MIPS reporting, providing physicians with a reliable and efficient tool to help them comply with MIPS regulations.





